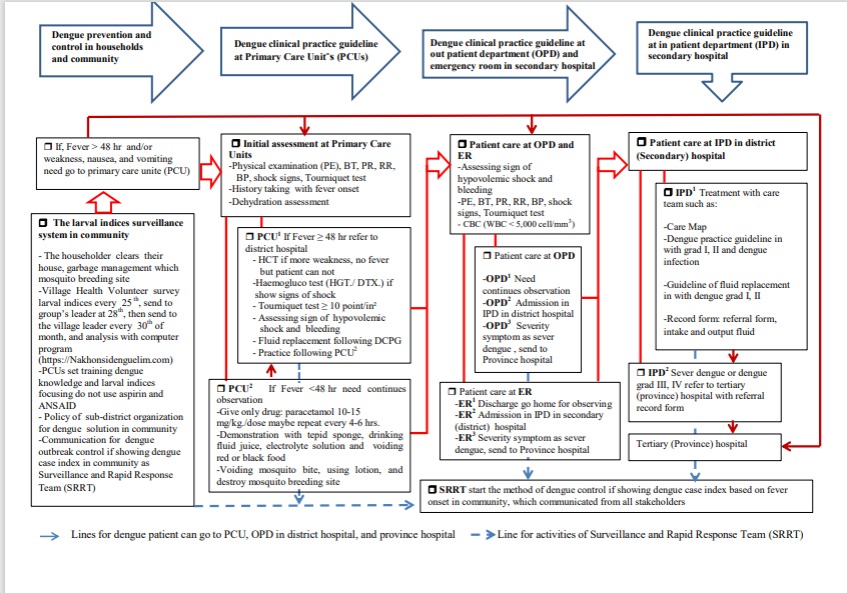
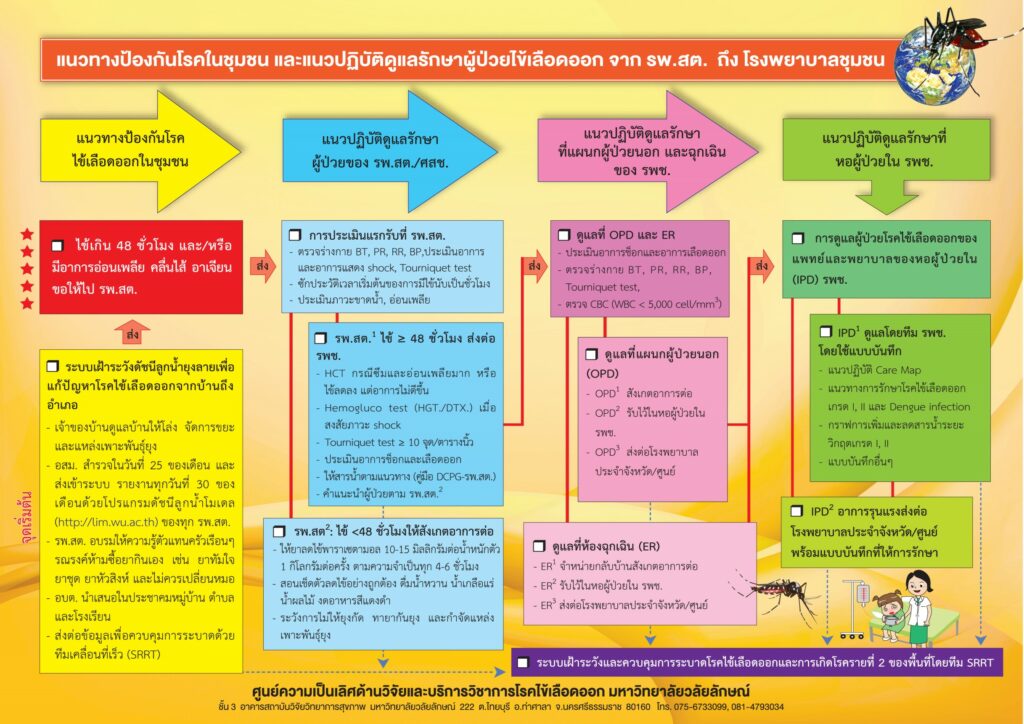
DPCG from household to PCU and the district hospital
After the using of DPCG, the guideline was concluded as the four steps dengue patient from household to district hospital.
First step: DPCG at household was the dengue prevention and control and basic care in household. The step was self-care with dengue prevention in the community. This step focused on dengue prevention with the larval indices surveillance system in the “Lansaka model”, which consisted of seven steps in 44 villages [19]. The system focused on the householder clearing their house and garbage management. Mosquito breeding site-village health volunteer surveys larval indices were performed on the 25th of every month, sent to the group’s leader on the 28th, then sent to the village leader on the 30th of month, who analysed them with a computer program (http: //Nakhonsi.denguelim.com). PCUs use training dengue knowledge and larval indices to eliminate mosquito breeding sites and avoid non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and aspirin. The dengue solution policy of sub-district organization was conducted in communities and schools. There was communication for dengue outbreak control information that showed a dengue case index in the community as the Surveillance and Rapid Response Team (SRRT).
The second step: DPCG at the PCUs. The guideline was patient have fever lasted > 48 hrs. and/ or weakness, nausea, and vomiting were present, the patient needed to go to the primary care unit. There were two patterns: 1) PCU1 refers to a district hospital if fever ≥ 48 hrs. Health care providers need to test (1) Hct. If weakness increased, and there was no fever, (2) the haemogluco test (HGT./DTX.) was performed; if the patient showed signs of shock, (3) the tourniquet test ≥ 10 points/in² was performed; (4) assess signs of hypovolemic shock and bleeding, (5) fluid replacement following DPCG, and (6) practice following PCU2. 2) PCU2 needs continuous observation if fever <48 hrs., (1) give only paracetamol 10-15 mg./kg./dose, may be repeated every 4-6 hrs., (2) demonstration with tepid sponge, drinking fluid juice, electrolyte solution and voiding red or black food, and 3) avoiding mosquito bite, using lotion, and destroying mosquito breeding site.
The third step: DPCD at OPD and ER in the district hospital. Patient care at the OPD and ER for assessing signs of hypovolemic shock and bleeding included PE, BT, PR, RR, BP, shock signs, tourniquet test, and CBC (WBC< 5,000 cell/mm3, platelets <100,000 cell/mm3). There were two options in OPD and IPD in that each channel was divided into 3 patterns: Dengue patient care at OPD consisted of 1) OPD1: for dengue patients, health assessment and screening were needed for advising and continuing observation; 2) OPD2: health assessment and DHF diagnosis for admission to IPD in district hospitals; and 3) OPD3: health assessment showed severe signs and symptoms as DSS and the patients were sent to tertiary (province) hospital.
Dengue patient care occurred in the ER when dengue patients visited the hospital from 16.00 pm. to 8.00 am. There were three patterns: 1) ER1 pattern was health assessment and discharge to go home for observing dengue signs and symptoms, 2) ER2: taking health assessment and diagnostic DHF for admission to the IPD in the district hospitals, and 3) ER3 pattern was a health assessment and diagnosis of dengue with severe symptoms and sending them to the tertiary hospital.
The fourth step: DPCG at IPD of the district hospital. There were two patterns that consisted of 1) IPD1 treatment with a care team, such as Care Map, as the dengue practice guideline in grades I and II and dengue infection, guideline of fluid replacement in dengue grades I and II, and filling out referral form and recording intake and output of fluid, 2) the IPD2 pattern was a guideline for severe dengue or dengue grades III and IV, which are referred to province hospital with the referral form. The guidelines for dengue prevention and control in the community and practice guidelines in primary- to the tertiary care (province) hospital (Maharaj Nakhon Si Thammarat hospital) need to be integrated and communicated to all stakeholders. Moreover, SRRT needs to monitor the outbreak situation at the case index of dengue fever in the community as community mobilization and perform outbreak activity as soon as the case index of fever is known.
The application of DPCG covered eight PCUs and the district Hospital. The dengue high morbidity rate of the district in 16 weeks was 124 cases/100,000 populations and there was no mortality rate. However, the DPCG’s record form of the PCUs needs to be completed. Finally, the new lines of dengue patient care were from the household to PCU and the district hospital, and they can possibly go to the tertiary hospital.
